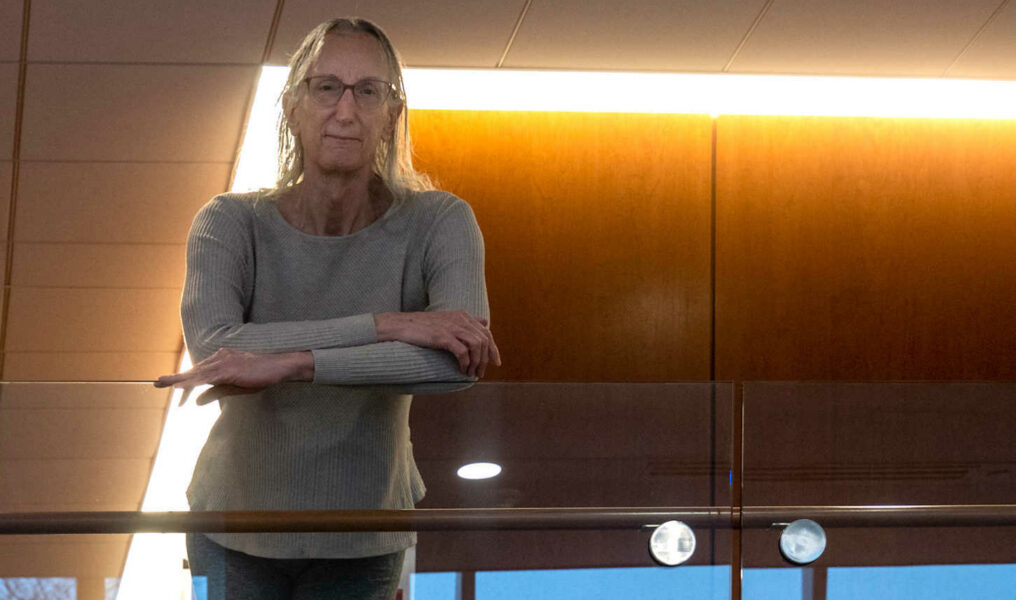
As a professional drummer, Rikki Bates knows something about keeping time. And time, over the past year, has moved at an agonizing tempo.
"You've got to go straight up the trail and, you know, cut down trees with nail files. It just takes a long time," she says. "Well, the clock's ticking."
Bates was 4 years old when she knew she wanted to play drums. Around that same time, she also realized she was different. Something felt wrong. "I felt paralyzed … I lost interest in absolutely everything and just felt like I wanted to die," says Bates, who lives in Cape Code, Massachusetts.
At last, in March 2020, she had access to a surgery she had known she wanted since she first heard of it in the 1970s. At 66 years old, she was finally ready to set a date for a gender-affirming operation that would drastically improve the quality of her life.
Then, the coronavirus hit, and the whole world paused.
"To think that I was all ready to have this facial surgery and then [to] have the rug pulled out from under me was devastating," says Bates. "It's terrible."
She had no choice but to keep doing what she had been doing for as long as she can remember — wait. During a stressful and traumatic pandemic year for everyone, she wasn't the only trans person to do so. Many transgender individuals seeking gender-affirmation surgery faced the additional stress of postponed lifesaving treatments.
Gender-affirmation surgeries can be a pivotal stage in a person's transition. Doctors today have surgical techniques at their disposal that make it safe and feasible to alter parts of the body to better align with a person's true gender identity.
Commonly sought procedures include bottom surgery (below the belt), top surgery (waist up) and facial surgery, where parts of the skull that serve as gender cues are altered. Not all people who are transgender choose surgery, but some feel that one or a combination of these surgical interventions is necessary for them to live their most authentic lives.
In Bates' case, she had already received three gender-affirming operations before the pandemic: two bottom, one top. For her, the surgeries made life worth living.
"Before I had any surgery, I just didn't care about anything anymore. I just didn't care about anything at all and just didn't want to be alive," Bates says.
After the surgery, everything changed. "I felt like this mountain of lead weights just went away," she says, "and never came back."
At every step of the way, she had to fight her insurance over the medical necessity of gender-affirmation surgeries for her, a process that dragged on "at a snail's pace" through months and years. But she never considered giving up because "it's the only path toward me being able to love myself, which isn't easy if you're transgender."
Last March, at the beginning of the pandemic, operating rooms across the nation shuttered their hermetically-sealed doors to any surgeries that were elective or nonessential. That included gender-affirmation surgeries, along with anything else that didn't require immediate and urgent medical attention.
Some operating rooms started performing nonessential surgeries during that summer, only to close once again when COVID-19 cases peaked this past winter. During a tumultuous year, trans people waiting for their surgery date were on an emotional roller coaster.
During this period, Amy Hunter, the executive director at OutFront Kalamazoo, an educational and advocacy group that provides support for LGBTQ+ youth who are experiencing homelessness, witnessed an uptick in demand for OutFront's therapy groups. This pattern is emblematic of how rough the past year has been for the trans community.
"The whole idea that gender-affirming care is elective needs to be disabused," says Hunter, a woman who is transgender. "In most cases, it's actually life-saving."
Hunter, 61, lives in Kalamazoo, and she said the area is "luckier than a lot of places across the state," and certainly across the country, because there are a few doctors there that specialize in gender-affirming care.
"It's really a hit or miss, whether you can find competent care or even a doctor that will see you," she says. This struggle to attain compassionate health care from a competent provider can take a toll on trans patients as they seek care.
"The process is slow," Hunter says. "We have to teach our doctors. We have to teach our social workers. We have to teach the intake people about who we are, and what our needs are and why. We try to teach those systems how to deal with us as who we really are, not as how they would perceive us [or] how they would like to perceive us."
Even areas where gender-affirming care is more easily found are not without their problems, and many people in trans or gender-nonconforming communities feel left behind, especially given the particular set of challenges posed by the last year.

Candace Nguyen works at Fenway Health in Boston as a clinical coordinator for STI and
HIV prevention clinics. Photo: Taylor Blackley
Candace Nguyen, 28, works at Fenway Health in Boston as a clinical coordinator for STI and HIV prevention clinics. Fenway Health recently marked its 50th year of providing healthcare to the LGBTQ+ community of Boston and beyond. Around 15 percent of the patients they care for are transgender or gender-nonconforming. For Fenway, ensuring a gender-affirming healthcare experience where patients feel safe and understood is a priority. After all, Nguyen understands firsthand the anxiety of waiting to express herself. She, like many of the other providers at the clinic, is a woman of trans experience.
"The fact that you have to wait to do that, I think that's more painful," she says. Nguyen started her transition at 25. She had only been on hormone therapy, which in her case suppresses male hormones (testosterone) and supplies her body with the female equivalent (estrogen), for a year when COVID-19 hit.
"I had this irrational fear that when COVID-19 happened the world was gonna end before I actually got to fully live my life," says Nguyen. "I don't want to feel like I wasted my whole life not living."
Quarantining at home with family, she felt disconnected from her community and her identity.
"Every day I would just be waking up, looking at myself in the mirror, and it [was] like, 'I'm not happy with myself. I'm not happy with the body that I am,'" Nguyen says.
The process of transitioning looks different for everyone. Regardless of whether people have surgery, they are not defined by the form their body takes.
"Whether or not folks medically transition, our spirit and our character stays the same," she says.
Now that she's seeing results from her hormone therapy, she feels like she's living for herself: "I'm finally like what I've always wanted to be, and I definitely feel much happier and more confident."
Ngyuen's colleagues in the behavioral health department are mental-health experts, many of whom are themselves intimately familiar with the experience of navigating the world as a person who is gender-nonconforming. For many providers, the pain of the past year hit close to home.
"There's been a really drastic impact by the start of the pandemic on lots of folks who are trans and nonconforming," says Annie Crossman, an outpatient psychotherapist.
Crossman has noted an extreme increase in their patients' anxiety and depression over the past year, with more people seeking help for their mental health and experiencing symptoms of mental illness.
Crossman, 28, provides mental health counseling at Fenway Health. They have been working from home over the past year in an apartment they share with their partner in Brookline, Massachusetts. Many of the people Crossman works with are from populations marginalized based on their racial, socioeconomic, ability and HIV/AIDS status, among other factors.
Crossman largely attributes the abundance of patients seeking treatment to social isolation and the postponement of gender-affirming treatments.
"A lot of folks have been staring at the calendar for quite some time and no longer have access… it gave a lot of people hope to have those surgeries scheduled," says Crossman. She worried about the trans people who have already been waiting years to receive treatment, and hoped the additional pandemic-related delays would not dissuade people from continuing their medical transition.
For Bates, this hardship was nothing new. She had been waiting for her place in the operating room for close to five decades. "There's just constantly one delay after another, after another, after another. It starts to feel like I'm just beating my head against the wall and this is never going to happen," she says.
She spent nearly a decade in court to secure her rights to transition-related medical care. Represented by lawyers from the New England-based GLBTQ Legal Advocates & Defenders, she appealed against her insurance, MassHealth, and its decision not to cover her transition-related care. This happened three times.
At every turn, there seemed to be another obstruction.
"Just trying to figure out all of it, getting all of these details to work, it was totally maddening," says Bates. Finally, in 2014, she had the coverage she needed after former Gov. Deval Patrick directed MassHealth to provide coverage for hormone therapy and gender-affirmation surgery.
Before COVID-19 shut everything down, Bates had an appointment with Dr. Branko Bojovic at Massachusetts General Hospital to schedule the first in a series of several facial-feminization surgeries. Her desired result after plastic surgery is a softer, more traditionally feminine appearance. This process is a huge undertaking, and in her case will include breaking, recontouring and reconstructing several parts of her skull.
"This is not about me expressing my gender how I want to," says Bates. "This is about me being stuck in this thing that I was born into that was never, ever, ever fun and something that I would never, ever, ever, ever wish on anybody else."
This procedure, while still considered plastic surgery, is not cosmetic. It has the potential to profoundly impact her life. Ideally, patients and their providers work together to select the best treatment options.
"They're not something that is emergent, but I do think of them as procedures that are urgent for many people and lifesaving for many people," says Dr. Robert Goldstein, the medical director of the transgender health program at Massachusetts General Hospital.
According to Goldstein, many patients experience a delay in finding the care they desire before coming to his clinic. These delays can range from a year or two up to 20 or 30 years. They can result from relatively minor administrative errors, like paperwork going back and forth between insurance and providers. In other cases, they are the effect of the patient experiencing discrimination as they sought treatment.
Once a patient has initiated the process, depending on the surgery that person wants, the first opening could be six months, a year or even two years away.
"These are surgeries that are highly desired, and unfortunately, there's only so much space in the operating room on any given day," says Goldstein.
On March 25, Bates underwent a frontal sinus setback, the first in a series of about five facial-feminization surgeries she plans to have done at Massachusetts General Hospital. Her recovery is going better and quicker than she could have hoped. "I only felt really bad for a couple of days [after] this past surgery," Bates says. "I've had years of torture, and that's way worse."
On April 16, Bates returned to have the stitches removed, and was already feeling more healing than discomfort. The changes are subtle, but for Bates, the transformation is profound.
"I really feel whole," she says. "I feel my forehead. I can feel what he did. And it's just so much softer and rounder and it just feels really good. I feel like I'm coming home."
A thin pink scar that traces the edge of her hairline, the faint memory of the surgeon's blade, is already fading. Even though there are a multitude of incisions still planned, more bones to be shaved and more flesh to be surgically altered in order to achieve her desired result, Bates has reason to hope that the most painful part of the process — waiting to live authentically, waiting to feel comfortable in her own body, waiting to receive healthcare that is gender-affirming — is nearly over.
"I still got a whole bunch more surgeries to go, but the goal is about to get reached," says Bates. "There's been all these other delays along the way, and I'm still working, chipping away at some of this mountain that's still left. But, you know, I can see that there's sunlight up there."